An electrocardiogram (ECG) is one of the simplest and fastest tests used to evaluate the heart. Electrodes (small, plastic patches that stick to the skin) are placed at certain spots on the chest, arms, and legs. The electrodes are connected to an ECG machine by lead wires. The electrical activity of the heart is then measured, interpreted, and printed out. No electricity is sent into the body.
An electrocardiogram records the electrical signals in the heart. It’s a standard and painless test used to detect heart problems and monitor the heart’s health quickly. An electrocardiogram — also called ECG or EKG — is often done in a health care provider’s office, a clinic, or a hospital room. ECG machines are standard equipment in operating rooms and ambulances. Some personal devices, such as smartwatches, offer ECG monitoring.
Natural electrical impulses coordinate contractions of the different parts of the heart to keep blood flowing the way it should. An ECG records these impulses to show how fast the heart is beating, the rhythm of the heart beats (steady or irregular), and the strength and timing of the electrical impulses as they move through the different parts of the heart. Changes in an ECG can be a sign of many heart-related conditions.
Some reasons for your doctor to request an electrocardiogram (ECG) include:
To look for the cause of chest pain. To evaluate problems that may be heart-related, such as severe tiredness, shortness of breath, dizziness, or fainting. To identify irregular heartbeats. To help determine the overall health of the heart before procedures such as surgery or after treatment for conditions such as a heart attack (myocardial infarction, or MI), endocarditis (inflammation or infection of one or more of the heart valves), or after heart surgery or cardiac catheterization. To see how an implanted pacemaker is working. To determine how well certain heart medicines are working. A baseline tracing of the heart’s function during a physical exam may be used to compare future ECGs and determine if there have been any changes.
An electrocardiogram is a painless, non-invasive way to help diagnose many common heart problems. A health care provider might use an electrocardiogram to determine or detect:
* Irregular heart rhythms (arrhythmias)
* If blocked or narrowed arteries in the heart (coronary artery disease) are causing chest pain or a heart attack
* Whether you have had a previous heart attack
* How well specific heart disease treatments, such as a pacemaker, are working
You may need an ECG if you have any of the following signs and symptoms:
* Chest pain
* Dizziness, light-headedness or confusion
* Heart palpitations
* Rapid pulse
* Shortness of breath
* Weakness, fatigue, or a decline in the ability to exercise
Usage of ECG Machine:
Before placing your ECG electrodes, it is essential to prepare the subject’s skin by wiping the chest area thoroughly with skin cleansing (alcohol) swabs. This removes any oil that may be on the patient’s skin, which can cause drift in your ECG/EKG signals. Once the skin is clean, find and mark the placements for the electrodes. Find and mark the correct lead placements for the ECG. Find the correct lead placement for the chest leads, starting with V1 and V2. It is essential to correctly place V1 and V2 because the remaining chest leads are placed in relation to these. To determine the placement of V1 and V2, feel to identify the top of your subject’s sternum. Approximately 4 centimetres below this, there is a ridge. This identifies the second intercostal space. Feeling down, you will come across the third and fourth intercostal spaces. Use a skin-safe marker to mark the fourth intercostal space as V2. Mark V1 in the mirror position on the opposite side of the chest.
You can do this by identifying V4 and V6, then filling in V3 and V5 as outlined below…V4 can be found in one intercostal space lower than V2, in line with the middle of the clavicle. Mark V4 with your skin-safe marker. Next, track along the torso to the subject’s left to find V6 at mid-auxiliary on the same horizontal level as V4. Mark V6.V5 can be marked at midway between V4 and V6. Likewise, mark V3 midway between V2 and V4. You should now have 6 marks for V1 to V6. Apply your electrodes to your 6 marks! The 6 electrode wires can now be connected to your recording device.
Apply lead 1 to the left arm. We suggest the front of the left shoulder be placed where there is little muscle or muscle movement to avoid any EMG signal disturbance. Next, apply lead 2 to the right arm. Again, the front of the shoulder is suggested here, in a place with little or no muscle or movement. Then, connect the left leg. Place the electrode slightly above the ankle. This electrode placement is the reference for all of the augmented leads. Finally, apply the “common” on the right-hand side ankle. This connects to the ground input on your recording device. Connect the limb leads to your recording device and test if you are receiving a signal.
Maintenance of the ECG Machines:
Regular cleaning and sanitization of the ECG machine’s external surfaces, electrodes, cables, and leads are essential to prevent the buildup of dirt and germs. Disinfecting the equipment helps reduce the risk of cross-contamination between patients and maintains a hygienic environment in the healthcare facility. Inspecting ECG cables and leads is necessary to identify any signs of wear or damage. Damaged cables or leads may result in poor signal quality or signal loss during recordings. Regular inspection helps detect issues early, allowing for timely replacements and preventing potential disruptions during patient examinations. For portable or battery-operated ECG machines, routine battery maintenance is essential. Ensuring that batteries are charged and functioning correctly helps prevent unexpected power failures during critical procedures and ensures continuous operation. Updating the ECG machine’s software is essential to ensure that it is running the latest firmware and features. Software updates often include bug fixes, security enhancements, and improved functionalities, enhancing the overall performance and reliability of the machine. The electrode gel used in ECG recordings can dry out over time, leading to poor signal conductivity. Regularly replacing the electrode gel ensures optimal signal quality and reduces the likelihood of recording artifacts.
When to change accessories:
Most ECG machines will function well for years if they are given the proper care and maintenance. However, there are some signs that an individual may need an ECG Machines replacement. These include frayed wires connecting the electrodes to the primary evidence of wear on the electrode heads-repeated error signals on the display unit (refer to the machine’s user manual for troubleshooting and assistance advice)-printer errors on the test graph including smudges, blank lines, or ink spots-printer feed errors or constant paper jams-inconsistent readings or a failure to read the electronic signals.
If any of these problems are occurring with the ECG machine, consider an ECG machine replacement. The good news is that new models are constantly being developed with improved accuracy, readings, and functions to enhance testing capabilities.
Best practices for comfortable Use:
Ensure the patient is reclined in a comfortable resting position. Ask them to lie still, remain quiet, and breathe normally while taking the ECG, as any skeletal muscle activity will be picked up as interference. Make sure you are using a high-quality ECG electrode, such as the AMBU SUPA tab, which can help to reduce the common problems associated with poor electrode adhesion. Ensure correct electrode placement by downloading and printing our free MG Medicare ECG placement guide as an easy reminder of where the electrodes should be positioned on the patient’s chest and limbs. It is usually recommended to record the ECG in a 4 x 3 format with a rhythm strip along the bottom of the ECG trace. This is usually lead II. If the patient has any clinical signs during the procedure, such as chest pain, then this should be recorded in the notes or on the ECG tracing itself. Ensure that the electrodes are removed from the patient’s skin once the ECG has been completed and dispose of them in the clinical waste. If you are not using an integrated device, such as our range of i3 integrated solutions, then make sure that the ECG is correctly labelled with the patient’s details. For more advice when taking a resting ECG, visit our MG Medicare ECG Tips page and keep an eye on our News section for the latest hints and tips. Remember, if you experience any problems with any of your Numed diagnostic or waiting room equipment, then we have a dedicated support section that can provide help and advice about a range of our equipment.
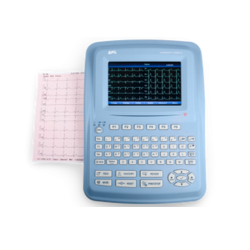
Top 5 ECG Machines In India
- BPL Cardiart 9108 ECG Machines
- Nidek 712 ECG Machines
- BPL Cardiart 9108D ECG Machine
- BPL Genx 3 ECG Machine
- Nidek 703 ECG Machine
